Semen Analysis
Your physician will likely order a semen analysis prior to either fertility treatments or semen storage. At CRBI, a typical semen analysis will determine the number of sperm cells present in the ejaculate (semen concentration), the percent of the cells that are moving (percent motility), the quality of movement associated with the sperm (e.g., good forward progressing, circular swimming, twitching movement or nonmotile) and the morphology of the sperm structures (e.g., shape and size of head and tail). In order to provide an accurate sample, patients are asked to abstain from ejaculation 2-7 days prior to producing the sample. To ensure that the sample can be quickly analyzed before a loss in quality, patients are asked to collect a semen sample in our private on-site collection room adjacent to the laboratory. Other parameters of semen that are examined include the volume of the ejaculate, color, liquid consistency of the semen (viscosity), the alkalinity of the semen (pH) and cellular and noncellular debris presence. The results from the semen analysis will help your physician decide on the best infertility treatment plan for you as well as diagnosing any underlying problem that may need further evaluation by a urologist.
Semen Cryopreservation
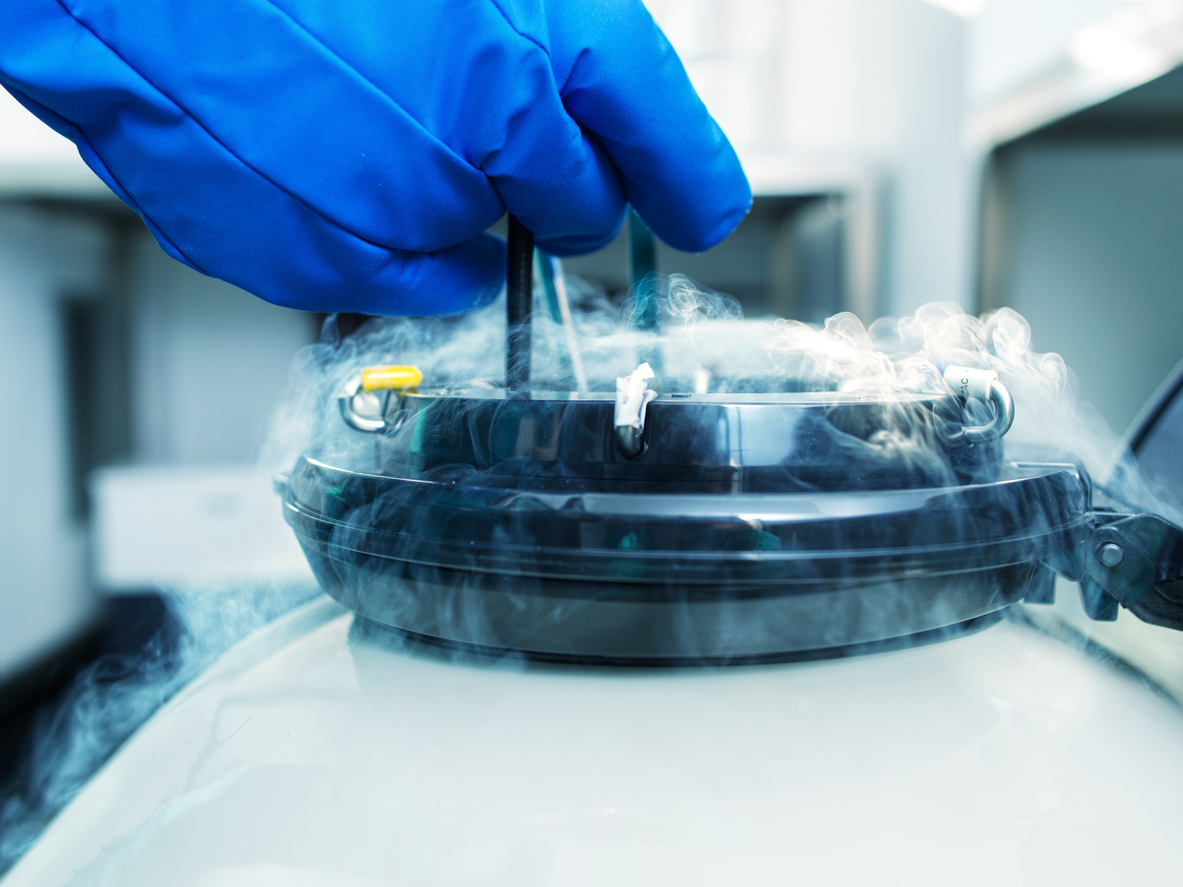
Cryopreservation is a freezing method that allows storage of samples for future use. Advances in freezing technology allow the preservation of fragile reproductive material, including oocytes, sperm, and embryos. Semen is added to a liquid medium that is protective for the freezing process. This mixture is placed in small vials and slowly cooled. Storage is provided in liquid nitrogen at -196 degrees C. At this low temperature, the semen can be stored for many years. There are many reasons why cryobanking sperm might be useful. Give our lab a call today if you think it might be a good option for you and/or your partner.
Cryopreservation of Surgically Obtained Sperm
MESA, PESA, TESA/TESE
Surgical Treatment of Male Infertility
Many factors contribute to male infertility, including age, nerve damage, erectile dysfunction, and physical obstructions of the reproductive tract. Also, severely low sperm numbers (or absence of sperm) in the ejaculate will significantly impair the ability to conceive. If the male reproductive tract is blocked, other means may be necessary to retrieve viable sperm. Several procedures aspirate sperm from the epididymis, where mature sperm can sometimes be found. Percutaneous epididymal sperm aspiration (PESA) is minimally invasive and can be done under local anesthesia. Micro epididymal sperm aspiration (MESA) is slightly more involved. If sperm are not found in the epididymis by PESA or MESA, the testes may be explored by testicular sperm aspiration/extraction (TESA/TESE). Other options might include collecting sperm during other procedures such as vasectomy reversal or varicocele repair surgery.
Cryopreservation of Surgically Obtained Sperm
Viable sperm obtained from any of these procedures are processed and cryopreserved by the laboratory for use in future IVF procedures. Specialized surgical procedures, such as those outlined above, are performed in collaboration with the care team at Urology of Indiana who specialize in male infertility.
In Vitro Fertilization
What is In Vitro fertilization (IVF)?
In Vitro Fertilization is a treatment for infertility due to a variety of diagnoses, including but not limited to ovulatory dysfunction, tubal blockage, endometriosis or low sperm count. Eggs and sperm are placed together in a nutrient-rich medium and are kept in an incubator that controls temperature, humidity, carbon dioxide and oxygen concentrations to closely mimic the environment of the fallopian tube, the area in the female reproductive tract where fertilization naturally occurs.
In Vitro Fertilization is only one assisted reproductive technique that may be recommended to treat infertility. Before any treatment occurs, a couple should have a multi-step diagnostic workup to determine which infertility treatment is most likely to be effective.
What procedures can I expect if I choose IVF treatment?
Ovarian Stimulation. Typically, your physician will prescribe a regimen of medications that are taken daily for a period of 10-12 days to stimulate your ovaries to produce many eggs. This treatment phase is called controlled ovarian stimulation and requires frequent monitoring of blood hormone levels as well as transvaginal ultrasounds to track follicular growth. From these tests, your physician will know when you are ready for the egg retrieval. Thirty-six hours before your egg retrieval is scheduled, you will take a medication to induce the final maturation of your eggs.
Ultrasound-guided Egg Retrieval
Egg retrieval is an outpatient surgical procedure. You will receive conscious sedation for this procedure. You may have your partner or other support person with you for the egg retrieval. Your physician will insert an aspiration needle through the vaginal wall to reach the ovaries. Your physician will "retrieve" the eggs from your ovaries into a sterile tube that is then passed to the embryologist, who identifies and washes each egg. The egg retrieval is normally completed within 20-40 minutes. The embryologist quickly transfers each egg to a nutrient-rich fertilization medium. You will typically be discharged after one to two hours after the retrieval.
What happens in the laboratory?
(View the 5 day development of embryos)
Typically, the semen sample is provided by the partner the same day as the egg retrieval. However, if semen was cryopreserved ahead of time, then semen processing would include thawing on the day of the egg retrieval. Some patients may choose to use an anonymous donor from a commercial sperm bank, or a known (directed) donor as their sperm source. Anonymous and directed-donors are required to undergo rigorous infectious disease testing (and six-month quarantine and retesting) before the specimen can be used for IVF.
At a specific time, the eggs are combined with sperm by an embryologist. The semen sample is prepared by the lab, and the fertilization process begins. After overnight culturing in an incubator, the eggs are examined microscopically to determine if normal fertilization has occurred.
Fertilization assessment
Determination of the fertilization status of the egg is one of the most critical steps of the procedure. A normally fertilized egg will contain 2 structures inside the egg called pronuclei that can be observed with a microscope. The presence of two pronuclei in the egg is indicative of normal fertilization. Greater numbers of pronuclei can occur if the egg is abnormally fertilized (e.g. polyspermy), and these abnormally fertilized eggs seldom result in normally developing embryos. It is important to separate normally fertilized from abnormally or unfertilized eggs at this step so that only embryos developing from normally fertilized eggs are used for embryo transfer to produce a healthy pregnancy. You will be called by one of our embryologists that day, and we will go over your fertilization report with you and of course allow you to ask any questions you have at that point.
Embryo culture.
The fertilized egg begins to divide (cleave) within about 12 hours after fertilization is observed. Embryos can sometimes be transferred to the uterus at this stage. However, it is often desirable to continue culture for two additional days to allow the embryo to reach a more mature (i.e. blastocyst) stage of development. In the body, the embryo is usually at the blastocyst stage when it arrives in the uterus. And having the embryos in culture for that extended period gives the lab additional information on each growing embryo. This information helps us select the embryos for transfer with the greatest potential for starting and maintaining a healthy pregnancy.
Embryo transfer.
A fresh embryo transfer is usually planned for day 5. The physician and patients are given an update by the lab. Based on the day 5 report and the couple's medical histories, the physician will make a recommendation to the couple regarding the appropriate number of embryos to transfer to optimize the likelihood of pregnancy while minimizing the risk of a multiples gestation. The embryologist then prepares the embryos for transfer by placing the embryos in a uterine catheter. The physician uses an ultrasound to guide the placement of the catheter containing the embryos into the uterine cavity. When placement is correct, the embryos are expelled from the catheter into the uterus. The embryologist checks the catheter to make sure no embryos are retained within the catheter. After rest for about an hour, the patient is discharged to her normal routine. The patient continues taking progesterone supplements to support the pregnancy until the physician recommends discontinuation. The pregnancy test is performed at about nine days after the embryos are transferred to the patient's uterus.
Intracytoplasmic Sperm Injection (ICSI)

Intracytoplasmic sperm injection (ICSI), gives patients with extremely low numbers of motile sperm another option in addition to the use of donor sperm. ICSI can be used for couples with a variety of diagnoses, but the most common reason is when severe male factor infertility is present (e.g. very low sperm numbers or very low sperm morphology results on a recent semen analysis).
Since only very few sperm cells are needed for ICSI, it is possible to use epididymal or even testicular sperm for fertilization of eggs, if ejaculated semen is not available. Sperm cells from any of these sources can be cryopreserved (frozen) for use in a future treatment cycle. Besides severely low sperm numbers, other common indications for ICSI include previous failed fertilization during an IVF cycle, or egg factors such as defects which allow more than one sperm to enter the egg.
The ICSI procedure involves the same ovarian stimulation and egg retrieval as conventional in vitro fertilization (cIVF). However several additional steps are required to prepare the eggs and sperm for ICSI. The eggs are exposed briefly to an acidic medium in order to remove the cumulus cells surrounding the egg, and this allows the embryologist to identify and select mature eggs for injection. The processed sperm cells are placed in a viscous solution that slows the sperm down, and this allows the embryologist to select and immobilize one good-quality sperm for injection into each egg.
Preimplantation Genetic Testing (PGT)

Preimplantation Genetic Testing screens an embryo’s quality at the chromosomal and genetic level. It can be especially helpful for a patient who knows they are at a high risk for passing on an inheritable genetic disease to their potential offspring. PGT can sometimes provide information that might help identify the healthiest embryos to transfer, but it is not recommended/necessary for all our patients. Talk to your REI about whether PGT might be a beneficial addition to your IVF treatment. And as always do not hesitate to give us a call if you have lab-related questions about PGT.
If your physician requests PGT as part of your cycle, CRBI will plan to perform biopsy of the trophectoderm (TE) cells from the embryo at the blastocyst stage (i.e. day 5 or 6 after the egg retrieval). Immediately after the biopsy, the cells are sent to a specialized PGT laboratory that performs the genetic analysis. The embryos are cryopreserved and stored at out facility until we receive a report back from the PGT lab. At that time, we review the PGT results with you and your physician, and then decide on a follow up plan including if/when to perform an embryo transfer.
Our Reference Genetic Laboratory for PGT:
CooperGenomics, A CooperSurgical company: www.coopergenomics.com
Assisted Hatching
Hatching out of the zona pellucida is required in order for the embryo to make contact with the recipient's uterine lining and begin the process of implantation. Usually, the embryo breaks through the zona on its own. But in some cases, assisting the hatching process can be helpful. If assisted hatching is warranted, an opening is created in the zona pellucida to facilitate hatching. This opening is created by using a laser.
Vitrification
Eggs and embryos are cryopreserved (frozen) using a technique called vitrification. Vitrification is a rapid-freeze method that cools the egg or embryo to -196 degree C almost immediately. This quick cooling reduces the chance for intracellular ice crystals to be formed, thus decreasing the degeneration of cells upon warming for use. Eggs and embryos are stored in liquid nitrogen. And at such extremely cold temperatures, cellular activity is essentially brought to a halt, and this allows the eggs or embryos to remain viable for years to come.